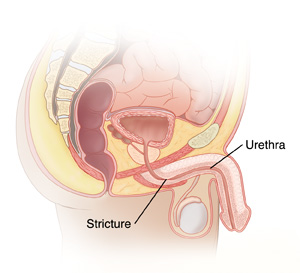
Urethroplasty is surgery to treat a narrowing (stricture) of the urethra. In men, the urethra carries pee (urine) from the bladder out of the body through the penis. It also carries sperm from the testicles, seminal vesicles, and prostate gland through the penis. The urethra may have a stricture that blocks the normal flow of pee. As a result, pee can back up in the kidneys and the tubes (called ureters) that carry pee from the kidneys to the bladder. This can lead to infection and kidney damage. Urethroplasty may be used to treat a stricture if less invasive (nonsurgical) treatments don’t work or aren't right for you.
Getting ready for surgery
Get ready for the surgery as you’ve been advised. Be sure to:
-
Tell your doctor about all medicines you take. This means prescription and over-the-counter medicines, as well as vitamins, herbs, and other supplements. Examples include warfarin and other blood thinners, clopidogrel, and daily aspirin. You may need to stop taking some or all of them before surgery. Don't stop taking any medicine on your own before your doctor tells you to.
-
Follow any directions you're given for not eating or drinking before surgery. This includes coffee, water, gum, and mints. If you've been instructed to take medicines, take them with a small sip of water.
The day of surgery
Urethroplasty takes about
Before the surgery begins
-
An I.V. (intravenous) line is placed in a vein in your arm or hand. This supplies fluids and medicine, such as antibiotics.
-
You may be given a medicine to prevent blood clots.
-
You'll be given general anesthesia to keep you from feeling pain during surgery. This medicine puts you in a deep sleep-like state. A tube may be inserted into your throat to help you breathe while under anesthesia.
During the surgery
-
Cuts (incisions) are made near the area that needs to be fixed. This may be in the skin between the scrotum and anus or on the penis.
-
The method used to fix the stricture is chosen based on the location and length of the stricture.
-
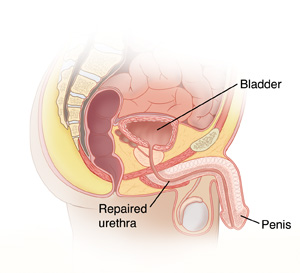
First, the stricture is cut out. Then the remaining ends of the urethra may be sewn together, called an anastomotic urethroplasty. Or the urethra may be fixed with skin and tissue taken from another part of the body, known as substitution urethroplasty. Tissue can be taken from the inside of your mouth or from the shaft of the penis.
-
In some cases, more than one surgery may be needed to fix the urethra. This is called a two-stage repair. Your surgeon can tell you more.
-
When the surgery is complete, the skin incisions are closed with stitches.
-
A thin tube (Foley catheter) is placed into your bladder. Another thin tube (suprapubic catheter) may be placed through a small incision in your belly (abdomen) and into your bladder. These tubes help drain pee until healing is complete.
Recovering in the hospital
After the surgery, you'll be taken to a recovery room. Here you’ll wake up from the anesthesia. You may feel sleepy and sick to your stomach. If a breathing tube was used, your throat may be sore at first. When you're ready, you'll move to your hospital room. While in the hospital:
-
You'll be given medicine to manage pain. Let your care team know if your pain isn't under control.
-
You’ll get up and walk as soon as you're able.
-
You’ll be taught coughing and breathing methods to help keep your lungs clear and prevent pneumonia.
Recovering at home
After your hospital stay, you'll be released to an adult family member or friend. Have someone stay with you for the next few days to help care for you. Recovery time varies for each person. Your doctor will tell you when you can return to your normal routine. Until then, follow the instructions you've been given. Make sure to:
-
Take all medicines as directed.
-
Care for your incisions as instructed.
-
Care for your catheters as instructed. Make sure nothing, such as clothing, pulls on the catheters.
-
Follow your doctor’s guidelines for showering. Don't swim, take a bath, use a hot tub, or do other activities that cause the incision to be covered with water until your doctor says it’s okay.
-
Don't do any heavy lifting and strenuous activities, as advised.
-
Wait
4 to 6 weeks before having sex. -
Avoid driving until your doctor says it’s okay. Never drive if you’re taking medicine that makes you drowsy or sleepy.
-
Wear a jockstrap for support, as directed.
-
Walk a few times each day. As you feel able, slowly increase your pace and distance.
-
Avoid straining to pass poop (stool). If needed, take stool softeners as directed by your doctor.
-
Drink plenty of water. This prevents pee odor and fluid loss (dehydration). Follow any other diet instructions you’re given.
When to call your doctor
Contact your doctor right away if you have:
-
A fever of
100.4 ° F (38.0 °C ) or higher, or as advised by your doctor. -
Symptoms of infection at an incision site, such as increased redness or swelling, warmth, worsening pain, or bad-smelling drainage.
-
Pain that can't be controlled with medicine.
-
Increased bruising or swelling of the penis or genital area.
-
Problems with the catheters.
-
Trouble peeing or no pee from your catheters for 4 hours.
-
Bloody pee with clots (Some pink-tinged pee is normal.)
-
Upset stomach (nausea) or vomiting that doesn’t go away.
-
Leg pain or swelling.
Call 911
Call
Follow-up care
You’ll have follow-up visits so your doctor can see how well you’re healing. Catheters will likely be removed after
Risks and possible complications
Risks of surgery include:
-
Bleeding. You may need a blood transfusion.
-
Infection.
-
Blood clots.
-
The stricture isn't fixed, or it comes back.
-
Pee leaking at the repair site.
-
Scarring of the urethra.
-
Problems peeing.
-
A change in how the penis looks.
-
A change in ability to ejaculate or have an erection.
-
Risks of anesthesia. The anesthesiologist or nurse anesthetist will discuss these with you.