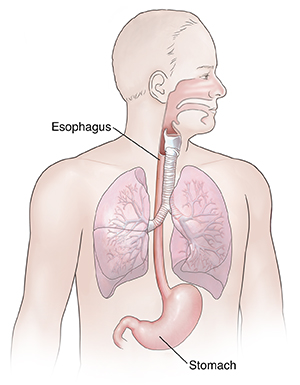
The esophagus is a tube that carries food from the mouth to the stomach. A valve (lower esophageal sphincter, or LES) prevents stomach acid from flowing upward. Sometimes this valve doesn't work correctly. Then stomach contents may flow back up (reflux) into the esophagus. When it happens again and again, it's called GERD (gastroesophageal reflux disease). GERD can irritate the esophagus. It can cause pain. It can also cause problems with swallowing or breathing. In severe cases, GERD can cause pneumonia that keeps coming back. This is from breathing in particles (aspiration) that are in the refluxed contents from the stomach. GERD can lead to other health problems, such as:
-
Inflammation of the lining of the esophagus (esophagitis)
-
Narrowing of the esophagus (stricture formation)
-
Cancer
Symptoms of reflux include burning, pressure, or sharp pain in the upper belly (abdomen). Symptoms may also be in the mid to lower chest. The pain can spread to the neck, back, or shoulder. You may have:
-
Belching (burping)
-
Acid taste in the back of the throat
-
Chronic cough
-
Sore throat
-
Increased salivation
-
Hoarseness
-
Trouble breathing
GERD symptoms often occur during the day after a big meal. They can also occur at night when lying down.
Home care
Lifestyle changes can help ease symptoms. Your healthcare provider may also prescribe medicines. Symptoms often get better with treatment. But if treatment is stopped, the symptoms often return after a few months. Most people with GERD will need to continue treatment. Or they may need treatment on and off.
Lifestyle changes
-
Limit or don't eat fatty, fried, or spicy foods. Also limit coffee, chocolate, mint, and foods with high acid content. These include tomatoes and citrus fruit and juices (orange, grapefruit, and lemon).
-
Don’t eat large meals, especially at night. Frequent, smaller meals are best. Don't lie down right after eating. And don’t eat anything 3 hours before going to bed.
-
Don't drink alcohol or smoke. As much as possible, stay away from secondhand smoke or passive smoke.
-
If you are overweight or obese, losing weight may help reduce symptoms.
-
Don't wear tight clothing around your stomach area.
-
If your symptoms occur during sleep, use a foam wedge to raise your upper body not just your head. Or place 4-inch blocks under the head of your bed. Or use 2 bed risers under your bed frame.
-
Talk with your provider if you have trouble making the suggested lifestyle changes. They may be able to give you resources to help.
Medicines
Medicines can help ease the symptoms of GERD. They also help prevent damage to the esophagus. Talk about a medicine plan with your healthcare provider. It may include 1 or more of these medicines:
-
Antacids. These help neutralize the stomach acids.
-
Histamine or H2 blockers. These decrease how much acid your stomach makes.
-
Proton pump inhibitors (PPIs). These medicines reduce how much acid is made better than H2 blockers.
-
Prokinetic agents. These speed up food digestion to lower the chance of reflux. They are generally prescribed along with H2 blockers or PPIs.
Take an antacid 30 to 60 minutes after eating and at bedtime, but not at the same time as an acid blocker. Try not to take medicines such as ibuprofen and aspirin. If you take aspirin for your heart or other health reasons, talk with your healthcare provider about whether you should continue taking it. Some people may need surgery for GERD.
Follow-up care
Follow up with your healthcare provider as advised.
When to seek medical advice
Call your healthcare provider if any of the following occur:
-
Stomach pain gets worse or moves to the lower right belly (appendix area)
-
Chest pain appears or gets worse, or spreads to the back, neck, shoulder, or arm
-
An over-the-counter trial of medicine doesn't relieve your symptoms
-
Weight loss that can't be explained
-
Trouble or pain swallowing
-
Frequent vomiting (can’t keep down liquids)
-
Blood in the stool or vomit (red or black in color)
-
Feeling weak or dizzy
-
Fever of 100.4ºF (38ºC) or higher, or as directed by your healthcare provider
-
Symptoms get worse or you have new symptoms